Exclusive interview with
Prof. Michele Brignole
Michele Brignole I Faint & Fall Programme I Department of Cardiology I IRCCS Istituto Auxologico Italiano I Ospedale San Luca I Milano, Italy
Professor Michele Brignole is the the coordinator of the Faint & Fall programme at the IRCCS Istituto Auxologico, Milan, Italy. He was formerly the Director of the Department of Cardiology of Ospedali del Tigullio, Lavagna, Italy. Prof Brignole’s main fields of research are diagnosis, pathophysiology, therapy of syncope and rhythm disturbances and catheter ablation of arrhythmias. He served as the chairman of the Guidelines on Syncope of the European Society of Cardiology (versions 2001, 2004, 2018) and chairman of the Guidelines on Cardiac Pacing and Cardiac Resynchronization Therapy of the European Society of Cardiology (version 2013). HealthManagement.org spoke to Prof Brignole on the importance of accurate syncope diagnosis and effective treatment and management strategies for this condition.
DIGITALK
You are currently viewing a placeholder content from Youtube. To access the actual content, click the button below. Please note that doing so will share data with third-party providers.
More InformationKEY POINTS
- Syncope is a frequent problem with nearly 40 to 50% of adults having experienced it once in their lives.
- While syncope is a benign condition in the majority of the patients, even benign syncope can have severe consequences in elderly patients.
- To date, the treatment of syncope is not very effective because it has not been personalised to the mechanism of the individual patients.
- These are the two mechanisms of non-cardiac syncope: hypotension and/or bradycardia.
- The prerequisite for the effective treatment of syncope is to determine the mechanism first and then treat accordingly.
FULL INTERVIEW
> Why is syncope an important topic, and how has awareness for syncope changed over the last few years?
Syncope is an important topic for two reasons. First, it is very frequent, and approximately 40% to 50% of adults have experienced a syncope episode once in their lives. Second, syncope has been perceived as a benign condition due to the high frequency. This is true for most patients with syncope who have a benign phenomenon that requires minimum attention and medical assistance. However, it is important to recognise that even benign syncope can have severe consequences due to falls and secondary trauma, fractures, intracranial haemorrhage and even death. In addition, syncope can alter a patient’s quality of life. This is especially true in older patients.
> What does a typical syncope patient look like?
It is hard to define a typical syncope patient and the features and characteristics because it is a heterogeneous condition. It is better to try and understand the mechanism of syncope and the risk for a syncope patient to develop serious consequences. In recent years, the focus has changed from looking at syncope as a marker of sudden death to seeing it as a predictor of severe trauma and poor quality of life. Very few patients of syncope are at risk of sudden death due to syncope, but a vast majority of patients at an advanced age are at risk of severe consequences.
> What are the challenges of diagnosing and managing syncope?
Older patients with syncope are at risk of secondary trauma. However, protecting these patients from the life-threatening consequences of this secondary trauma is not enough.

It is equally important to take action to prevent the recurrence of syncope. This requires aetiological diagnosis and a diagnostic workup to determine the true mechanism of syncope.
This is essential to initiate specific and effective treatment. To date, the treatment of syncope is not very effective because it has not been personalised to the mechanism of the individual patients. This is the challenge that must be overcome in the next few years.
> What diagnostic tools do you consider important for the proper diagnosis of syncope?
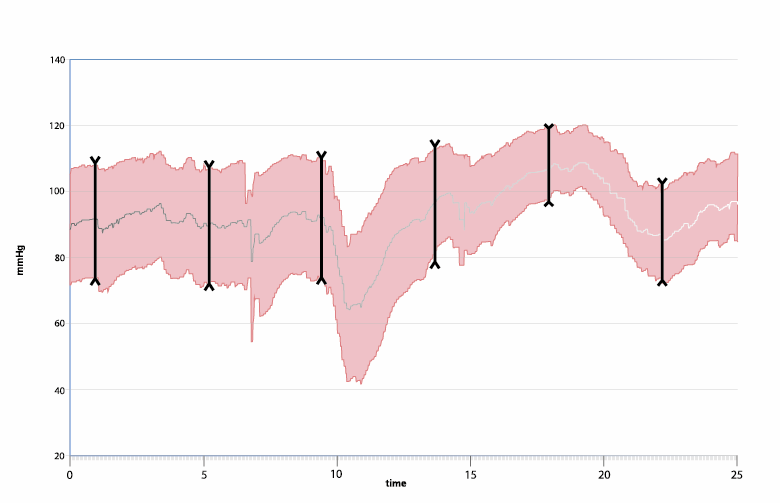
It is important to diagnose the mechanism of syncope rather than aetiology. It is also important to document what happens at the time of a syncope episode. This would involve knowing the blood pressure and the heart rate at the time of a syncope episode in order to determine the mechanism.
The ideal diagnostic test is to document the spontaneous syncope using electrocardiographic monitoring and documenting blood pressure. However, it can be difficult to measure blood pressure at the time of an episode. Electrocardiographic monitoring often requires the implantation of a loop recorder that cannot be performed in every patient.

An alternative solution is to provoke syncope artificially in a laboratory in order to understand its mechanism. Cardiovascular autonomic testing, namely active standing test, carotid sinus massage, tilt table test, vasovagal manoeuvres, and 24-hour ambulatory blood pressure monitoring (ABPM) can be useful in this situation.
> What are the international standards in assessing syncope?
The guidelines from the European Society of Cardiology (ESC) are very useful. I was the chairman of the last version of this guideline published in 2018, and I would encourage those interested to refer to these guidelines because they have recommendations for the management of syncope. These guidelines also include a practical section explaining what to do and how to manage a patient with syncope. There are also other guidelines from the American Heart Association (AHA) and the American College of Cardiology (ACC). There are excellent guidelines from the U.K. and national guidelines used in many countries in Europe, Japan and other regions. Clinicians can use any guidelines they prefer, but the important thing is to follow them when managing syncope patients.
> Where can a syncope patient turn to when they have the problem of fainting?
For the last 30 years, my colleagues and I have tried to write guidelines and editorials, do research, organise educational programmes and practical meetings, have face-to-face discussions with doctors etc. Unfortunately, the results of this effort are not what we enthusiastically expected. The major reason for this is that syncope is different from other diseases. In fact, syncope is not a disease. It is a symptom, and the symptom could be due to a different disease, and the disease could fall under the expertise of a different specialty. It is important to understand that some forms of syncope are neurological, some cardiological, some arrhythmic, and some due to blood pressure. There isn’t one expert who can deal with all these characteristics. Even if there was such an expert, they still don’t have the right instruments and tools to reach an accurate diagnosis. There is always something that we cannot do or some test that we cannot perform.

This situation leads us to conclude that the only way to treat syncope efficiently is to prevent its recurrence. In other words, the failure to treat syncope is a syncope recurrence, and the efficacy of syncope treatment is that there is no syncope recurrence. And in order to prevent syncope recurrence, it is important to establish dedicated facilities where syncope experts can do their job and are supported by the right equipment and tools, the right structure and the right personnel.
I strongly believe that creating a specialised structure can successfully prevent recurring syncope in a large majority of syncope patients. If we cannot prevent recurrence, we have failed.
> What are the treatment options after a syncope diagnosis?
The treatment of syncope cannot be guided by aetiology alone. It needs to be guided by aetiology plus the knowledge of the mechanism. For example, it is critical to know if an individual patient fainted because their blood pressure fell to a very low value or their heart stopped beating. These are the two mechanisms of any non-cardiac syncope. The prerequisite for the effective treatment of syncope is to determine the mechanism first and then treat it accordingly. For example, if syncope is due to lower blood pressure, the treatment should be focused on increasing the blood pressure. Conversely, if syncope is due to bradycardia, the treatment should be focused on increasing the heartbeat. This is the only way to achieve a high success rate in syncope patients. Otherwise, most patients will continue to have a recurrence, and many of these will suffer from serious fractures and other serious consequences resulting in disabilities and even death.
> What message would you pass on to syncope patients?
The vast majority of syncope is benign. Almost all syncopes occurring in young adults (< 40-50 years of age) in the absence of comorbidities or structural disease are benign. These patients have a very low risk of trauma secondary to syncope. Even those in the minority among this patient group who may be at risk of trauma can be easily identified and treated.
Therefore, most syncope patients do not need to be worried about their condition and can lead normal lives with education, preventive measures and reassurance. They don’t need any sophisticated investigation or assessment in a syncope unit. They can be easily treated by a general practitioner, cardiologist, neurologist or an internist. However, the very opposite is true for syncope in elderly patients. Syncope in elderly patients can be unpredictable. This patient segment is at a high risk of severe consequences in the event of a syncope episode, irrespective of the aetiology of syncope. Therefore, these patients should be referred to a syncope unit and evaluated carefully until the exact mechanism is established and treatment is initiated.
> What do you think is needed for a more effective syncope assessment?
My interest is to have tools that will be able to document blood pressure and heart rate at the time of syncope. Also, the use of remote technology and artificial intelligence could be utilised to improve syncope assessment.
At this time, it is very difficult and very rare to be able to measure blood pressure at the time of syncope. Measurement of blood pressure a few minutes after the end of a syncope episode is not useful. Therefore, if I had the option to ask the industry for one thing in the future, it would be to have a device that can measure blood pressure at the time of syncope. This is my most important requirement.
*References: