Diagnosing Initial Orthostatic Hypotension
Initial Orthostatic Hypotension (OH) is described as a rapid and transient drop in blood pressure associated with the increased risk of falls, fractures and syncope, especially in the ageing population. [1] As prevalence is high, the problem is evident, but due to limited access to reliable continuous diagnostic methods, the detection of OH is restricted. Experts demand continuous blood pressure measurements instead of the intermittent upper arm method with sphygmomanometers.
> Why are standard methods insufficient?
Can a disease such as OH, which is characterized by extremely rapid changes in hemodynamics, be efficiently diagnosed using standard methods such as upper arm blood pressure measurement? The answer is no! This has just recently been confirmed by a brand-new meta-analysis of the prevalence of initial orthostatic hypotension in adults aged 65 and older by Tran et al.
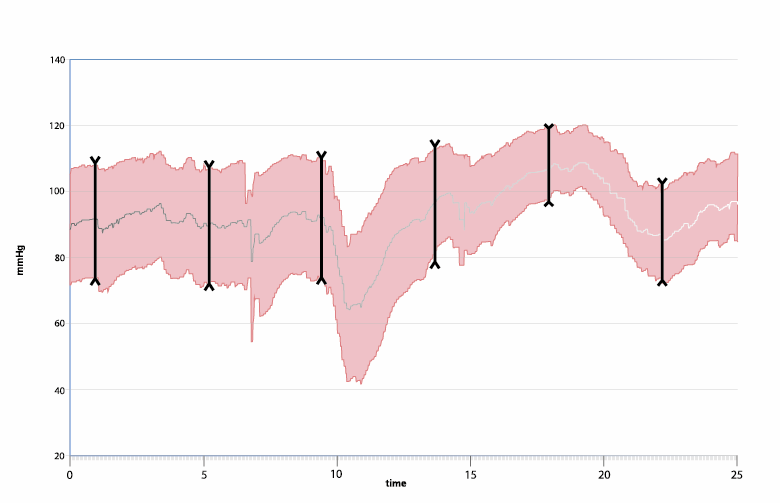
Data of more than 5,400 individuals underlines the insufficiency of intermittent blood pressure measurements to reliably diagnose OH, compared to continuous methods. In patients suffering from initial OH, systolic blood pressure drops to > 40mmHg or to > 20 mmHg in diastolic blood pressure within the first 15 seconds of Active Standing – a commonly used test to assess the cardiovascular response to standing.
The rapid blood pressure changes can hardly be detected with an upper arm sphygmomanometer. In fact, the pooled prevalence of continuously measured initial OH was five times higher than intermittently measured initial OH. “Continuous blood pressure monitoring is recommended to capture the transient changes in blood pressure upon immediate active standing or passive tilting.” [1]
> Demand for continuous methods
Other scientific data by Mol et al. also shows the need for continuous measurements in Active Standing Tests as “Orthostatic BP measurements using sphygmomanometer have an inadequate time resolution to record clinically relevant dynamics of orthostatic blood pressure recovery.” [2]
With regard to the negative implications such as pre-syncopal episodes or falls, the demand for continuous methods to reliably diagnose initial OH is evident. “There is a need to establish a consensus on the diagnosis of initial OH using continuous blood pressure devices to consistently identify participants with initial OH”. [1]
Esquivias et al. take on a similar notch when it comes to the efficient clarification of syncopal events. Many implications and costly test procedures might be saved if the recommendations of the ESC Syncope Guidelines, which include continuous blood pressure measurement in the course of tilt table testing (HUT), are taken into account right after initial assessment.
The experts evaluated the use of Head-up tilt test (HUT) in 1,058 patients with suspected vasovagal syncope (VVS) or orthostatic hypotensive syncope (OHS), after an adequate initial inconclusive evaluation. HUT was positive in 57.5% of all patients, 81% were identified with non-cardiogenic syncope, potentially avoiding a significant number of unnecessary diagnostic tests. [3]
The topic of a successful diagnosis of orthostatic hypotension (OH) and syncope is not restricted to the elderly only. “Orthostatic symptoms are common in children and adolescents such that 15% experience syncope at least once in teenage years.” [4] A review with 112 pediatric patients reports the successful application continuous blood pressure, heart rate and stroke volume measurement during HUT to identify orthostatic hypotension based on nonspecific symptoms such as headaches, pre-syncope, syncope, fatigue, abdominal pain, nausea, etc. [4]
> Reliable solutions available
These studies show that reliable non-invasive continuous blood pressure monitors have been on the market for a long time and have proven their importance for diagnosing syncope.
For initial orthostatic hypotension as described before, such tools do not seem to be the standard yet, although highly recommended by the experts: “Continuous BP measurements should be made routinely available and used in geriatric outpatient clinics.” [2]
A comprehensive implementation of this claim is now easier than ever:

CNSystems is launching the Touch Force® Touch CARDIO – the successor of the well-known Task Force® Monitor. It is an optimized solution for non-invasive hemodynamic measurement and includes the successfully established CNAP® technology. The device has especially been designed for an easy application in the area of syncope assessment.
Because every beat counts to win the race against sudden blood pressure drops!
References:
- Tran, J., Hillebrand, S. L., Lange, P. W., Iseli, R. K., Meskers, C. G. M., & Maier, A. B. (2021). Prevalence of initial orthostatic hypotension in older adults: a systematic review and meta-analysis. International Journal of Cardiology: Hypertension, 8, 1–9.
- Mol, A., Slangen, L. R. N., van Wezel, R. J. A., Maier, A. B., & Meskers, C. G. M. (2021). Orthostatic blood pressure recovery associates with physical performance, frailty and number of falls in geriatric outpatients. Journal of Hypertension, 39(1), 101–106.
- Barón-Esquivias G, Díaz Martín AJ, Del Castillo ÁM, Quintanilla M, Barón-Solís C, Morillo CA. Head-up tilt test diagnostic yield in syncope diagnosis. J Electrocardiol. 2020 Nov-Dec;63:46-50. doi: 10.1016/j.jelectrocard.2020.09.016. Epub 2020 Oct 11. PMID: 33075618
- Gourishankar, A., Belton, M. D., Hashmi, S. S., Butler, I. J., Lankford, J. E., & Numan, M. T. (2020). Demographic and clinical features of pediatric patients with orthostatic intolerance and an abnormal head-up tilt table test; A retrospective descriptive study. Pediatrics and Neonatology, 61(1), 68–74. https://doi.org/10.1016/j.pedneo.2019.06.012