CNAP® blood pressure
Bridging the gap between intermittent NBP and continuous invasive blood pressure
continuous
non-invasive
arterial pressure
CNAP® blood pressure is the core parameter and is measured beat by beat by means of the very easy-to-use and patented CNAP® finger sensor,
Standard NBP upper arm measurement can only provide intermittent snap-shots of the patient’s blood pressure status. With CNAP® the complete picture is available:
CNAP® finger sensor
Unique double-barrel design for a quick and easy application using innovative CNAP® technology measuring continuous blood pressure and providing advanced hemodynamic parameters.
- Slip-on design
- Simply to be placed on two adjacent fingers
- Immediately in the right position
- No need for additional fastening
- Reusable
- Intelligent technology comfortably embedded
- Infrared sensors, electronics and inflatable pressure chambers are placed in soft tubes located on the inside of both cylinders, ensuring comfortable fit.
- Automatic deflation of pressure chambers upon stopping the measurement makes removal of CNAP® finger sensor very easy.
- IP protected design: ideal for long-term measurements & stable position throughout the measurement
- The CNAP® finger sensor allows for switching the “measurement-finger” either at a predefined interval or even manually which makes measurements for up to 24 hours possible.
- Consistently stable position throughout the measurement: no shifting, no slipping out of position
- 3 different sizes available
VASCULAR UNLOADING TECHNIQUE
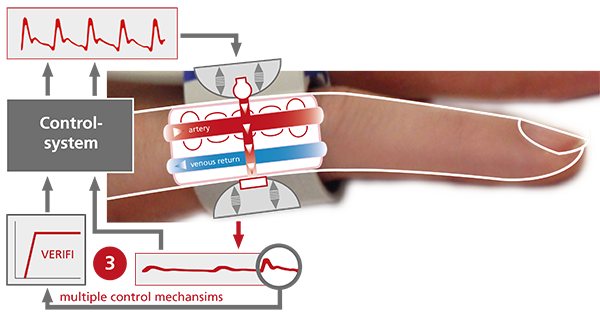
The CNAP® technology is based on the Vascular Unloading Technique, which goes back to the Czech physiologist Jan Peňáz in the 1970s.(1) It is the basic principle for detecting blood volume changes in the finger and transforming plethysmographic signals into continuous blood pressure information.
CNSystems has continuously improved this technology throughout the past decades.(2)
This is how it works:
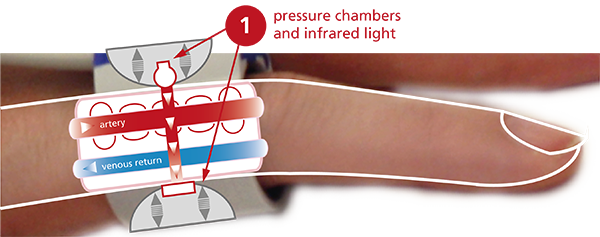

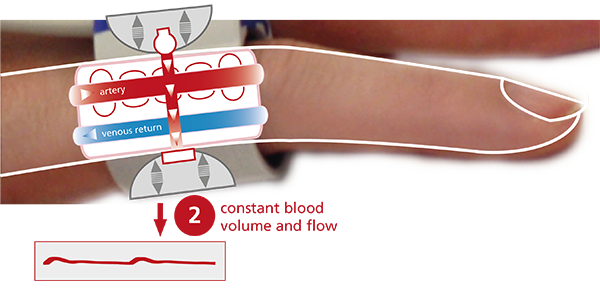
The blood flow in the finger is detected by infrared light sensors.
Pressure is exerted on the artery by inflating or deflating the integrated pressure chambers in order to “neutralize” blood pulsation and keep the blood flow constant.


ACCURATE & RELIABLE
A large number of validation studies confirm that CNAP® blood pressure measurement is highly accurate and comparable to invasive standards in various settings. (3,4,5)
OUR PRODUCTS PROVIDING CNAP® BLOOD PRESSURE
Get the full hemodynamic picture based on our CNAP® technology: non-invasive, continuous blood pressure, cardiac output, advanced hemodynamics and dynamic fluid parameters.
Non-invasive monitoring of blood pressure and advanced hemodynamics for medium and low-risk surgery.
Setting new standards for autonomic function testing and syncope assessment.
Hemodynamic measurement just got easier – integration or interfacing
References:
(1) Peňáz J: Photoelectric Measurement of blood pressure, volume and flow in the finger. Digest of the 10th international conference on medical and biological engineering – Dresden (1973).
(2) Fortin J et al: Continuous non-invasive blood pressure monitoring using concentrically interlocking control loops. Computers in Biology and Medicine 36 (2006) 941–957
(3) Jeleazcov et al. Precision and accuracy of a new device (CNAP) for continuous non-invasive arterial blood pressure monitoring: assessment during general anesthesia. British Journal of Anesthesia 2010 vol. 105 (3) pp. 264-72
(4) Ilies, C. et al (2015): Comparison of a continuous noninvasive arterial pressure device with invasive measurements in cardiovascular postsurgical intensive care patients: A prospective observational study. European Journal of Anaesthesiology, 32(1), 20–8
(5) Smolle KH, et al. The Accuracy of the CNAP® Device Compared with Invasive Radial Artery Measurements for Providing Continuous Noninvasive Arterial Blood Pressure Readings at a Medical Intensive Care Unit: A Method-Comparison Study. Anesth Analg. 2015 Dec;121(6):1508-16. doi: 10.1213/ANE.0000000000000965. PMID: 26496367.